Contraception in France: disparities in women’s use by income level
Press release Published on 22 November 2023
In France, the right to contraception is recognized as a fundamental component of sexual and reproductive health rights. However, a new study conducted by INED in collaboration with INSERM (Institut National de la Santé et de la Recherche Médicale) has revealed that even in a system that provides full health insurance coverage for women with low income, inequalities persist in the use of reimbursed contraceptive methods: a lower proportion of women at the bottom of the income scale use contraceptives than other women, at all reproductive ages. This study shows that lifting a financial barrier by reimbursing health care costs does not prevent other potential barriers from hindering access to contraception for women with low income.
|
KEY FINDINGS: —Only 36% of low-income women use reimbursed contraception, as against 46% of women with higher income; —The contraceptive methods used by low income women are different from those used by women with average or high income. For example, women with relatively little income aged 20 to 24 less often choose oral contraceptives (23%, as against 38% of other women in the same age bracket) and more often use contraceptive implants than higher-income women (respectively, 8% and 4%); —Women with low income aged 45 to 49 use the hormonal IUD method less often than other women in the same age bracket (respectively 6% and 14%). |
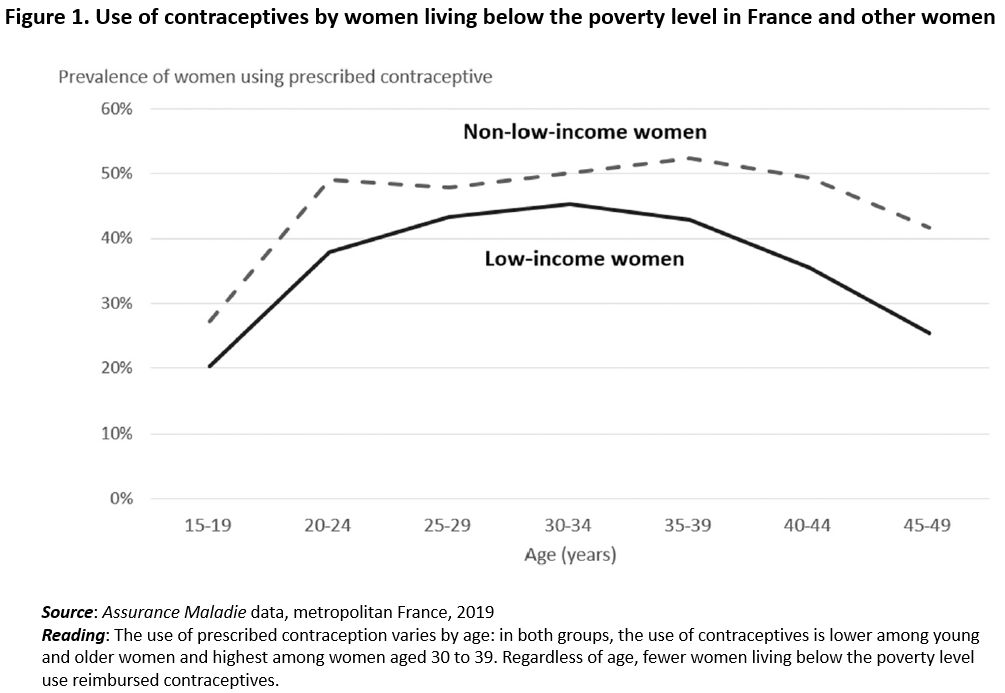
This study, which uses data from France’s Assurance Maladie universal health insurance system, analyzed data on 14.8 million women aged 15 to 49 living in France in 2019, 11% of them living below the poverty level. It took account of the main contraceptive methods reimbursed by the health insurance system: contraceptive implant, copper IUD, hormonal IUD, and reimbursed birth control pills. But despite guaranteed reimbursement, a lower proportion of low-income women use reimbursed contraceptives: 36%, compared to 46% of average- or high-income women. This disparity holds regardless of age (see Figure 1 below).
The study’s findings call into question the idea that financial cost is the sole obstacle to contraceptive use among low-income women. The observed differences may also be due to a number of non-financial barriers, including difficulty accessing contraceptive prescribers (getting a medical appointment, carrying out the formalities required to maintain health insurance coverage), which seems to lead women to turn to non-reimbursed contraceptives so as not to have to consult a doctor or midwife to obtain contraceptives.
The study results also show that contraceptive types varied widely between the two groups. A smaller proportion of low-income women aged 20 to 24 use oral contraceptives than of women with average or high income in the same age bracket (23%, as against 38%) and a greater proportion use implants (8%, compared to 4%). Meanwhile, proportionally fewer low-income women use hormonal IUDs (6%, as against 14%).
The study also found that contraceptive method differed by women’s income level—a result that may be explained not only as reflecting different choices but also by other factors. Low-income and young women are often targeted by public health programs promoting contraception in response to higher risks of an unwanted pregnancy in those categories. Consequently, health professionals may encourage lower-income women to use highly efficient contraceptive methods, such as the implant. Gaining access to a gynecologist may also be especially complicated for low-income women, and this may in turn explain the fact that few of them use hormonal IUDs.
A deeper understanding of the impediments to contraceptive use is essential if women are to be empowered to make informed choices about pregnancy timing and spacing. Though reimbursement for contraceptives is essential to guaranteeing equitable access to birth control for all, this study shows that other factors seem to play a decisive role in access to contraception.